Click on the boxes to see answers to common questions about upper endoscopy procedures.
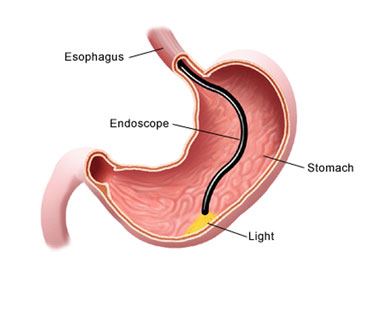
Upper endoscopy lets your doctor examine the lining of the upper part of your gastrointestinal tract, which includes the esophagus, stomach and duodenum (first portion of the small intestine). Your doctor will use a thin, flexible tube called an endoscope, which has its own lens and light source, and will view the images on a video monitor. You might hear your doctor or other medical staff refer to upper endoscopy as upper GI endoscopy, esophagogastroduodenoscopy (EGD) or panendoscopy.
Upper endoscopy helps your doctor evaluate symptoms of persistent upper abdominal pain, nausea, vomiting or difficulty swallowing. It’s the best test for finding the cause of bleeding from the upper gastrointestinal tract. It’s also more accurate than X-ray films for detecting inflammation, ulcers and tumors of the esophagus, stomach and duodenum.
Your doctor might use upper endoscopy to obtain a biopsy (small tissue samples). A biopsy helps your doctor distinguish between benign and malignant (cancerous) tissues. Remember, biopsies are taken for many reasons, and your doctor might order one even if he or she does not suspect cancer. For example, your doctor might use a biopsy to test for Helicobacter pylori, the bacterium that causes ulcers.
Your doctor might also use upper endoscopy to perform a cytology test, where he or she will introduce a small brush to collect cells for analysis.
Upper endoscopy is also used to treat conditions of the upper gastrointestinal tract. Your doctor can pass instruments through the endoscope to directly treat many abnormalities – this will cause you little or no discomfort. For example, your doctor might stretch (dilate) a narrowed area, remove polyps (usually benign growths) or treat bleeding.
An empty stomach is essential for an accurate and safe examination, so you should have nothing to eat or drink, including water, for approximately eight hours before the examination.
Our anesthesiologist will administer a short acting intravenous sedative and will be present to monitor your vital signs during the procedure. You will not experience any sensation of gagging or choking. A mouthpiece will be placed between your teeth to keep your mouth open and to prevent your teeth from biting our scope. You will lie on your left side, and the endoscope will be passed through your mouth and into the esophagus, stomach and duodenum. The endoscope doesn’t interfere with your breathing. The examination typically lasts 10 minutes.
You will be monitored until most of the effects of the medication have worn off. Your throat might be a little sore, and you might feel bloated because of air introduced into your stomach during the test. You will be given a liquid to drink before you leave our office. Once you leave the office, you will be able to eat unless you are instructed otherwise.
Your test results will be discussed with you before you leave. The biopsy results will take approximately 5 business days and you will be notified by phone by one of our nurses.
You will not be allowed to drive for 12 hours. You will need to arrange for someone to accompany you home because the sedatives might affect your judgment and reflexes for the rest of the day.
Although complications are rare, bleeding can occur at a biopsy site or where a polyp was removed. If this occurs, it’s usually minimal and rarely requires follow-up. Other potential risks include a reaction to the sedative used and a perforation (a tear in the gastrointestinal tract lining). It’s important to recognize early signs of possible complications. If you have a fever after the test, trouble swallowing or increasing throat, chest or abdominal pain, call us immediately.